
Every month, I have students who have had a cesarean birth ask me for “my thoughts on VBAC” or “Vaginal Birth after Cesarean Section.” Newest research states that each year 1.5 million childbearing women have cesarean deliveries, and that this population continues to increase.
The report adds stronger evidence that VBAC is a reasonable and safe choice for the majority of women with prior cesarean. Moreover, there is emerging evidence of serious harms relating to multiple cesareans. (Agency for Healthcare Research and Quality (US); March 2010.)
I asked my friend Marina if she could share her thoughts on VBACing:
Lisa: “Marina, as a patient with a prior cesarean section who successfully had a vaginal delivery after a cesarean (VBAC), would you encourage women in America to attempt to VBAC and why?”
Marina: “Absolutely! Recovery was so, so much easier! The bonding I was able to do right away was so much better…she latched right on and has always been a great nurser. Noah had respiratory issues, I’m sure from being a c-section and she just did so well!”

I have quite a number of friends who have successfully VBAC’d, their overwhelming concensus to the VBAC question is—“Just try to do it!” They all agreed, that if someone asked, they’d recommend a Trial of Labor for that Vaginal Birth After Cesarean Section because:
- There was NO MAJOR SURGERY- no side-effects like numbness, pain at the incision site, increased risks for bleeding or risks of infection
- It was safer for mom and baby
- VBAC reduces risks to mom should she have to undergo major abdominal surgery in the future
- They bonded with their babies as soon as they were born (with fewer transfers to transition nursery)
- Because babies went “skin-to-skin” immediately, most were able to nurse within the first 30 minutes of life.
- They had fewer breastfeeding challenges due to positioning problems because of an abdominal scar, respiratory problems with the baby or separation time from baby after birth
- Their stay in the hospital was shorter, they went home sooner.
- For most women, it was a true reconciliation of their past. It was the chance for them to let their bodies to do what they were meant to do—it allowed their hearts to heal from the emotional trauma of a cesarean section and to celebrate their ability to birth.
It’s not to say that having a vaginal birth was easy, but all would choose to VBAC again if they had the chance to, and some did.
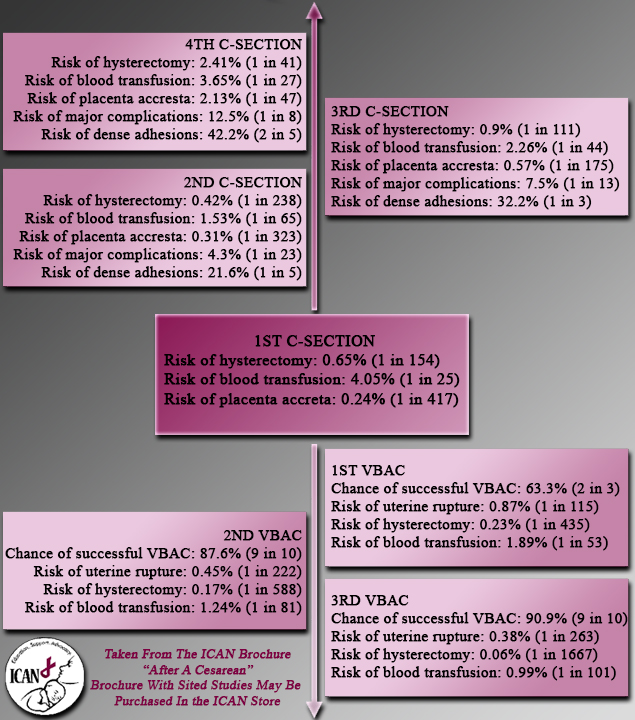
In 2010, the National Institutes of Health (NIH) reaffirmed the same information they had shared at their landmark 1980 summit on VBAC and shared that yes, VBAC labors have a very high rate of success for most women. ( NIH VBAC Consensus Statement) Approximately 60-80% of appropriate candidates who attempt VBAC will be successful. (ACOG Less Restrictive VBAC Guidelines) It does not mean that finding a care provider to support VBAC won’t be challenging or that you might not encounter difficulties, but you can make the choice for VBAC. This is why I love “ICAN” , the International Cesarean Awareness Network, organized to advocate for women who desire to have a vaginal birth after cesarean section (VBAC) or a trial of labor after cesarean section (TOLAC) and support them by giving evidenced-based research so that these women are informed of their choices to birth. Please check out their link for this information: International Cesarean Awareness Network
Also in 2010, the American Congress of Obstetricians and Gynecologists (ACOG) released updated practice guidelines for vaginal birth after cesarean (VBAC). ICAN hopes that the latest ACOG Less Restrictive VBAC Guidelines will enable women to find the support and evidence-based care that they need and deserve. Every woman must understand the capabilities and limitations of the care provider and facility she chooses– the facility and provider must have immediate access to an operative suite and immediate anesthesia coverage in the event or an obstetrical emergency, regardless of the minimal risk of a possible uterine rupture occuring (0.5-0.9%).
Less restrictive access to VBAC will lead to lower risks to mothers and babies from accumulating cesareans. The updated guidelines state that VBAC is a safe and reasonable option for most women, including some women with multiple previous cesareans, twins, and unknown uterine scars. ACOG also states that respect for patient autonomy requires that even if an institution does not offer trial of labor after cesarean (TOLAC), a cesarean cannot be forced nor can care be denied if a woman declines a repeat cesarean during labor.
Childbirth Connection states that the “bottom line” for deciding on whether you should attempt to have a vaginal delivery after a cesarean depends on whether or not you have a clear and compelling need for a repeat cesarean, if not, a VBAC is:
- Safer for you in pregnancy
- Safer for you and your babies in subsequent pregnancies.
However, it is not without risks, including:
- Scar giving way: The scar is more likely to give way during a VBAC labor than in a repeat c-section; for most women (exceptions noted below), the added risk of the scar giving way is about 4.2 in every 1,000 VBAC labors. In other words, nearly 238 women would need to experience the risks involved with repeat c-section to prevent one uterine rupture during a VBAC labor.
- Death of baby: While the scar giving way poses a threat to the baby, the added risk that the baby will die from a problem with the scar during a VBAC labor, compared with women planning repeat c-sections, is about 1.9 in every 10,000 VBAC labors. In other words, over 5,200 women would need to experience the risks involved with repeat c-sections to prevent the death of 1 baby due to uterine rupture. This is compared to the overall perinatal mortality rate of 6.64% regardless of delivery method. (CDC- National Vital Statistics System)
- Hysterectomy in mother: If the scar gives way, some women have an urgent hysterectomy (removal of the uterus). However, cesareans also increase risk for urgent hysterectomy, and women who plan a VBAC are not more likely to experience an unplanned hysterectomy than women planning repeat c-section.
- Multiple scars in uterus: As the number of c-section scars increases, the risk for experiencing several serious problems increases for women and fetuses in future pregnancies and births. These include:
- scar rupture in a subsequent labor
- ectopic pregnancy: the embryo develops outside the uterus
- placenta previa: the placenta grows over the cervix, the opening to the uterus
- placental abruption: the placenta separates from the uterus before the baby is born
- placenta accreta the placenta grows abnormally into or even through the uterus.
- The following factors do not increase risk of the scar giving way during labor:
- type of uterine scar not known
- low vertical uterine incision for prior c-section (may have been used if c-section was performed earlier in pregnancy before growth in lower part of the uterus)
- baby estimated to be large, and to weigh more than 4,000 grams (8 pounds, 13 ounces)
- pregnancy goes past 40 weeks, and labor is not induced
- The following factors are associated with a low risk of the scar giving way, but too few cases have been studied to know the true risk:
- twin pregnancy: uterine rupture does not appear to be more common in twin VBAC labors compared with singleton VBAC labors
- use of external cephalic version: turning a baby who is positioned buttocks- or feet-first (breech) to head-first position by manipulating the woman’s belly does not seem to cause or be associated with uterine rupture
As you consider these risks, keep in mind that on average, 3 out of 4 women who labor after a c-section will give birth vaginally with care that encourages and supports VBAC (and fewer than 1 in 100 will experience the scar giving way). Even in cases where women are told they have a low chance of having a VBAC, if given the chance many or even most give birth vaginally.
- Check out www.vbacfacts.com and www.childbirthconnection.org they have the best compilation of VBAC research to date!
Though the risk of uterine rupture is low—less than one percent—it is the major cause for concern in VBACs. “How will I know that I’m experiencing a dehiscence of my uterine scar?” is the question I’m asked frequenty. Signs and symptoms, though subtle, may become quite obvious and would indicate the need for an emergency cesarean section immediately:
- Changes in fetal heart rate: Prolonged, late, or recurrent variable decelerations or fetal bradycardias are often the first and only signs of uterine rupture. Bujold and Gauthier showed that abnormal patterns in fetal heart rate were the first manifestations of uterine rupture in 87% of patients. Overall, in 4 studies from 1983-2000, prolonged decelerations of fetal heart rate or bradycardias occurred in 114 (80%) of 143 cases of uterine rupture. This is the one reason why continuous fetal monitoring is indicated, so that changes can be observed if they occur.
- Abdominal pain and tenderness. 5% of women experiencing uterine dehiscence complained of abdominal pain. The pain may not be severe; it may occur suddenly at the peak of a contraction. The woman may describe a feeling a sharp pain at the incision site, that it “gave way” or “ripped.”
- Chest pain, pain between the scapulae, or pain on inspiration—Pain occurs because of the irritation of blood below the woman’s diphragm
- Hypovolemic shock caused by internal bleeding—Falling blood pressure, tachycardia, tachypnea, pallor, cool and clammy skin, and anxiety. The fall in blood pressure is often a late sign of hemorrhage
- Cessation of uterine contractions.
Conclusion: Recognize that attempting a vaginal delivery after a cesarean section is not without risks, however, the success rate of having a vaginal birth are in your favor especially if you spontaneously go into labor on your own. Even if you don’t have spontaneous labor and the option is an induction of labor, an induction may still result in a vaginal birth outcome. Cochrane Database published a study stating, “When a woman has had a previous caesarean birth, and requires induction of labour in a subsequent pregnancy, there are two options for her care: elective repeat caesarean or planned induction of labour. Both forms of care have benefits and risks associated with them. There were no trials to help women, their partners and their caregivers make this choice.” This information is to empower you with knowledge to give you a clearer understanding of the benefits and risks for VBACs; to help you recognize where your physicians are “coming from”; and to help you make informed decisions for the care you receive for a better birth outcome.
References
^ “Uterine Rupture in Pregnancy: eMedicine Obstetrics and Gynecology”. Retrieved 2010-03-23.
ACOG Practice bulletin no. 115: Vaginal birth after previous cesarean delivery. Obstet Gynecol. Aug 2010;116(2 Pt 1):450-63.
Bujold E, Mehta SH, Bujold C, Gauthier RJ. Interdelivery interval and uterine rupture. Am J Obstet Gynecol. Nov 2002;187(5):1199-202
www.cdc.gov accessed 30 August 2013.
www.childbirthconnection.org accessed 30 August 2013.
Coassolo KM, Stamilio DM, Paré E, Peipert JF, Stevens E, Nelson DB, et al. Safety and efficacy of vaginal birth after cesarean attempts at or beyond 40 weeks of gestation. Obstet Gynecol. Oct 2005;106(4):700-6.
Cochrane Database of Systematic Reviews. Elective repeat caesarean versus planned induction of labour for women with a previous caesarean birth. published: May 16, 2012 accessed: PubMed 30 August 2013.
Guise JM, Denman MA, Emeis C, Marshall N, Walker M, Fu R, Janik R, Nygren P, Eden KB, McDonagh M. Vaginal birth after cesarean: new insights on maternal and neonatal outcomes. Obstet Gynecol. 2010 Jun;115(6):1267-78.
www.improvingBirth.org accessed 30 August 2013
www.ICAN.org accessed 30 August 2013
Landon MB, Spong CY, Thom E, Hauth JC, Bloom SL, Varner MW, et al. Risk of uterine rupture with a trial of labor in women with multiple and single prior cesarean delivery. Obstet Gynecol. Jul 2006;108(1):12-20
National Institutes of Health Consensus Development conference statement: vaginal birth after cesarean: new insights March 8-10, 2010. Obstet Gynecol. Jun 2010;115(6):1279-95.
www.vbacfacts.com accessed 30 August 2013.